What to Expect: Amputation Surgery.
May 4, 2021 Leave a Comment
The following article offers a wealth of information concerning what to expect before, during, and after amputation surgery.
The most important goal of your entire treatment—from the operation to rehabilitation, to the fitting of your prosthesis—is to restore your mobility.
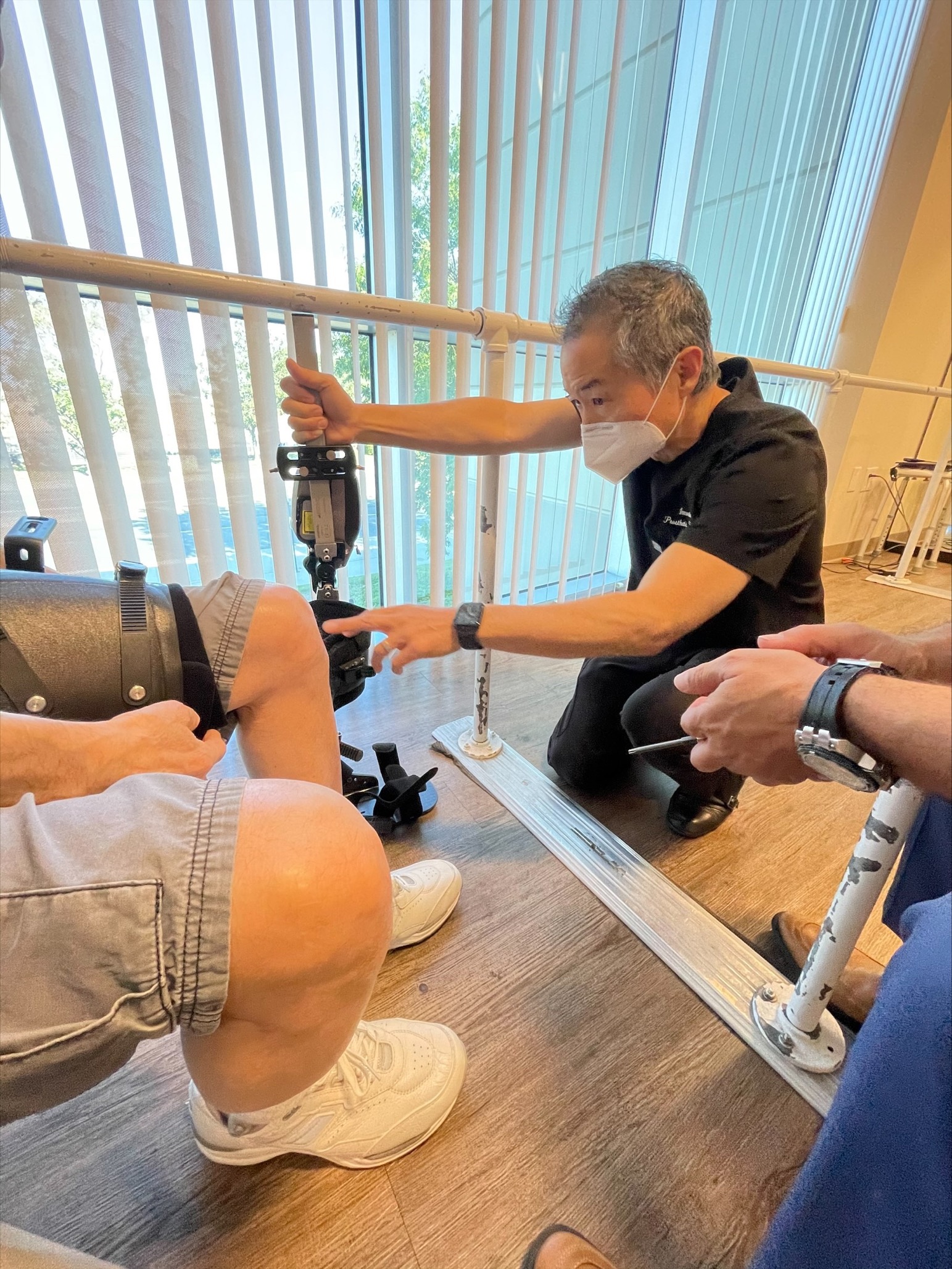
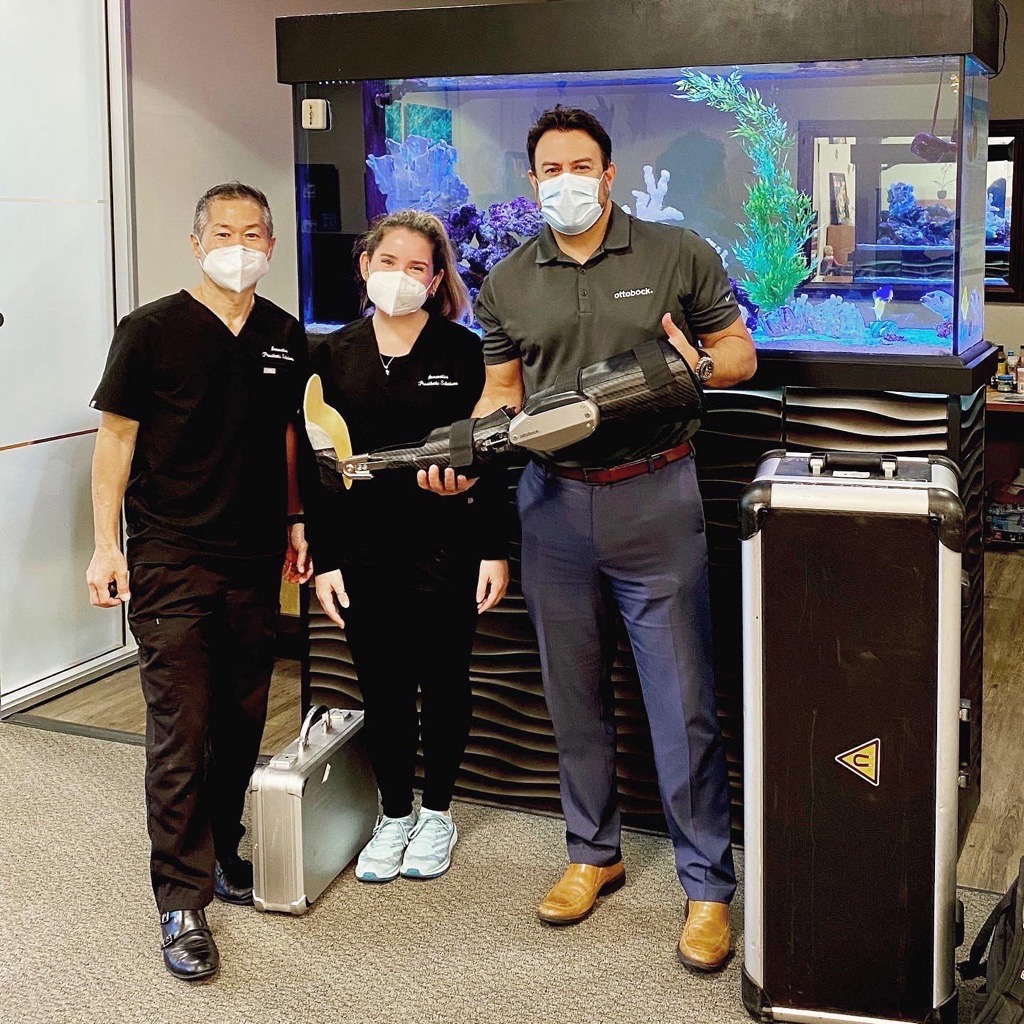
Your therapy team, which includes your doctors, therapists, prosthetists—and of course, you and your loved ones—will help you achieve the most independence possible, so that you can lead an active and mobile life. On average, this rehabilitation process takes between two to six months, although this can be affected by various factors, including your level of motivation and how well your prosthesis fits.
Whether you’ve known about your amputation surgery for a while, or just found out, remember that you’re not alone. Your treatment team is there to support you, answer questions—and find the best solutions for you.

Initial examinations
If you are to undergo planned amputation surgery, you will be examined in detail several times before the surgery. Your doctors will explain what will happen both during and after the operation. Of course, if you’ve had a traumatic accident, your conversations will occur after the surgery.
During these discussions, you have the opportunity to ask any questions which are important to you. It’s a good idea to take notes of what you want to ask the doctor before the discussions so that you don’t forget anything.
Psychological support

An amputation is a big change in your life and it may be helpful to get psychological counseling. Counseling can help you work through any issues or fears you may have.
Talking to other amputees
We also recommend that you talk with peers who have also undergone amputation surgery. It is good to hear how others deal with the situation, and in many cases they’ll also be able to share tips on everything from using your prosthesis to getting the right fit. Talk to your therapy team about how best to get in contact with peer support groups.
What does ‘amputation’ mean, and why is it done?
Amputation is described as the separation of a bone in healthy tissue or the removal of a limb at a joint (exarticulation).
Amputation surgery may be necessary if an injured or diseased limb is not expected to heal and if the patient’s life is endangered as a result. Possible causes include circulation issues, infections, accidents, cancer, or a congenital malformation of the limb. In these cases, it is usually known well in advance that an amputation will become necessary. In contrast, sometimes it is necessary to amputate unexpectedly, for example due to a severe injury after an accident.

What does ‘amputation level’ mean?
The term amputation level is used to describe the location at which the body part is amputated.
The amputation level is determined by the doctor before the operation and is based on the reason for the amputation. For planned interventions, a prosthetist is normally consulted as well in order to clarify which amputation level is suitable for subsequent fitting of the prosthesis.

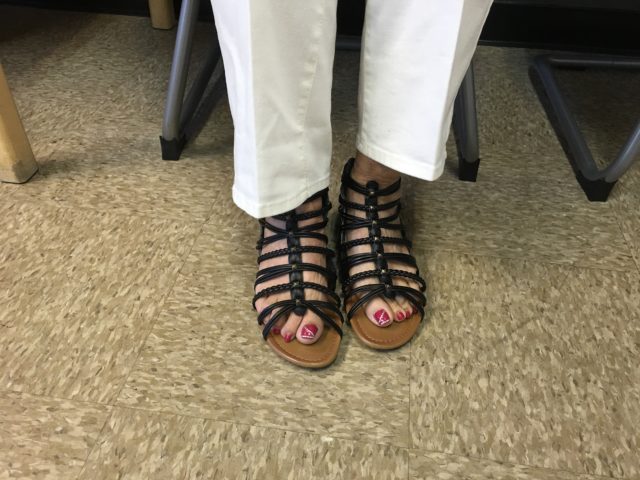
Foot amputation

Over twelve different amputation levels are common in the foot area. They range from a toe amputation to a metatarsal amputation or amputations in the tarsal area.
When there is less need for—or difficulty in fitting—a prosthesis that offers increased function, Cosmetic silicone prostheses are sometimes used.
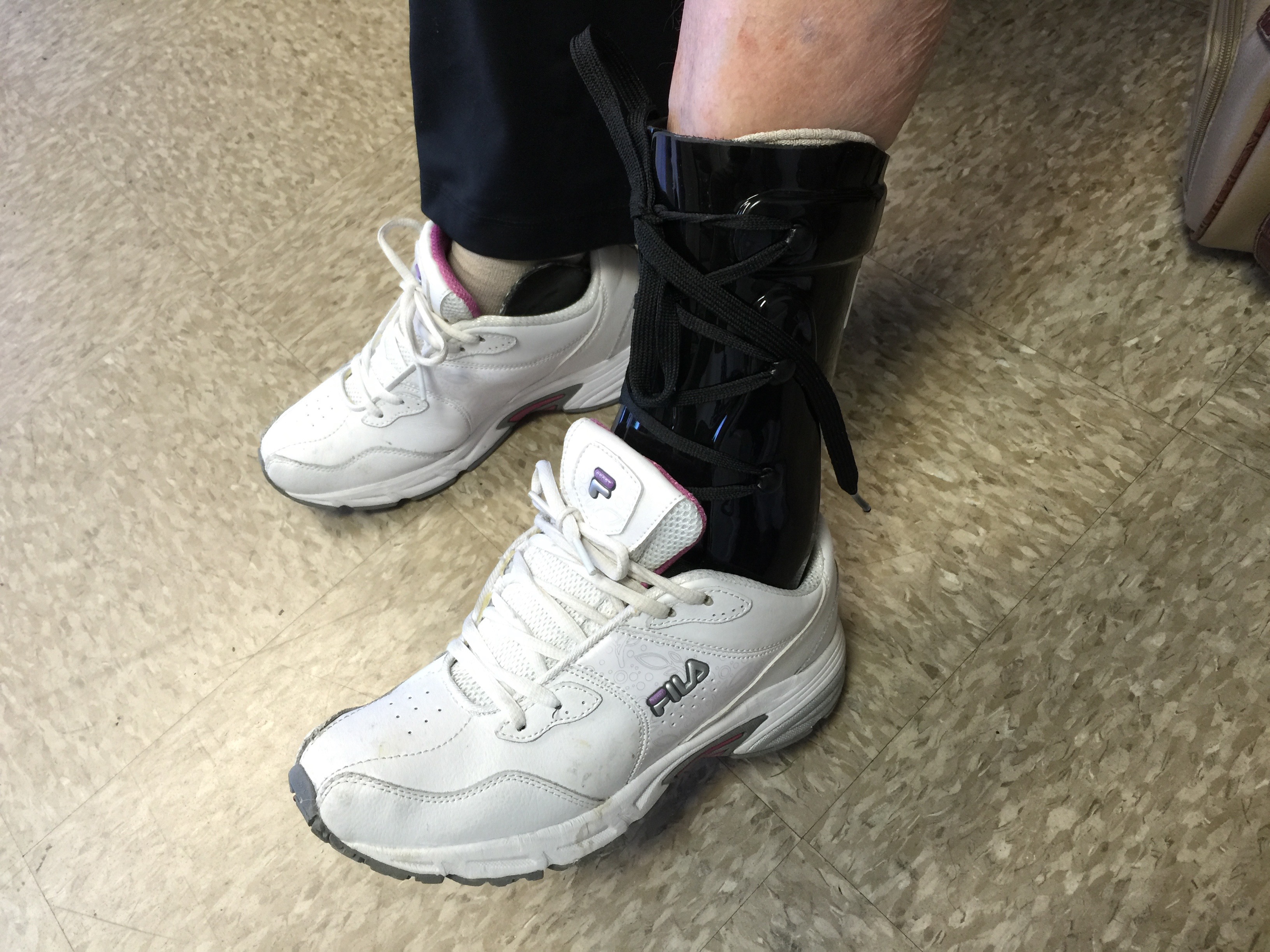
Transtibial amputation

For transtibial (also known as ‘Below the Knee’ or ‘BK’) amputations, the amputation occurs through the tibia and fibula bones of the lower leg.
The transtibial prosthesis consists of a socket, which contains the residual limb (the amputated limb, colloquially referred to as the ‘stump’), a prosthetic foot as well as adapters and connecting elements. Information on these products is available here. A prosthesis can be disguised with a cosmetic cover so that it is hardly noticeable visually.
Knee disarticulation
In knee disarticulation surgery the knee joint is separated and the lower leg is removed. The entire thigh is retained in the process.
The prosthesis consists of a socket, which contains the residual limb (the amputated limb, colloquially referred to as the ‘stump’), a prosthetic knee joint, and a prosthetic foot, as well as adapters and connecting elements. Information on these products is available here. A prosthesis can be disguised with a cosmetic cover so that it is hardly noticeable visually.
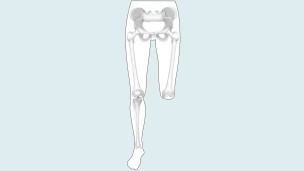
Transfemoral amputation
In a transfemoral amputation (also known as ‘Above the Knee’, or ‘AK’), the amputation occurs through the femur, or thigh bone, of the upper leg, so that the knee is no longer present.
The prosthesis consists of a socket, which contains the residual limb (the amputated limb, colloquially referred to as the ‘stump’), a prosthetic knee joint, and a prosthetic foot, as well as adapters and connecting elements. Information on these products is available here. A prosthesis can be disguised with a cosmetic cover so that it is hardly noticeable visually.
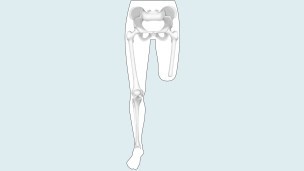
Hip disarticulation

During a hip disarticulation, the amputation is performed in the hip joint area. With this amputation the pelvis will be used to control the prosthesis later on.
The prosthesis consists of a socket, which contains the pelvic area, a prosthetic hip joint, a prosthetic knee joint, and a prosthetic foot, as well as adapters and connecting elements. Information on these products is available here. A prosthesis can be disguised with a cosmetic cover so that it is hardly noticeable visually.
Hemipelvectomy

In a hemipelvectomy, the entire leg, and part of the pelvis up to the sacrum are amputated. With this amputation the pelvis will be used to control the prosthesis later on.
The prosthesis consists of a specialized socket, which contains the remaining pelvic area, a prosthetic hip joint, a prosthetic knee joint, and a prosthetic foot, as well as adapters and connecting elements. Information on these products is available here. A prosthesis can be disguised with a cosmetic cover so that it is hardly noticeable visually.
After Amputation
Immediately after the operation, the focus will be on your recovery and the healing of your residual limb. Both are important so that you can start rehabilitation soon and be fitted with a prosthesis.